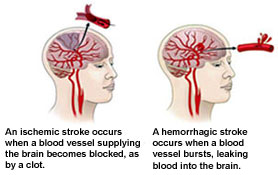
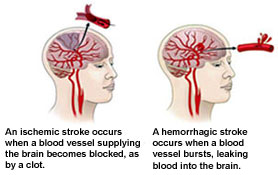
 According
to O’Sullivan, a stroke or cerebral vascular accident (CVA) is
defined as a sudden loss of neurological function caused by an
interruption in blood flow to the brain with neurologic deficits
persisting for greater than 24 hours. Strokes cause damage to brain
tissue. Clinical manifestations include changes in consciousness and
impairments in sensation, motor function, cognition, perception, and
language (1).
According
to O’Sullivan, a stroke or cerebral vascular accident (CVA) is
defined as a sudden loss of neurological function caused by an
interruption in blood flow to the brain with neurologic deficits
persisting for greater than 24 hours. Strokes cause damage to brain
tissue. Clinical manifestations include changes in consciousness and
impairments in sensation, motor function, cognition, perception, and
language (1).
Strokes are the most common cause of disability among adults in the
United States and affect approximately 700,000 individuals every
year (1). Following stroke, patients often have disturbed balance and
postural control leading to impairments in steadiness, symmetry, and
dynamic stability. This can cause problems in reactive postural
control and anticipatory postural control alike. The disruptions of
central sensorimotor processing make it difficult to adapt postural
movements to the changing demands of a task or environment.
Patients’ responses to destabilizing forces are frequently
insufficient and result in loss of balance and falls (1).
In fact, stroke is one of the greatest risk factors for falls in
elderly people. Incidence rates of falls have been reported between
23% and 50% in studies of people with chronic stroke (>6 months
post-stroke) in comparison to only an 11%-30% incidence rate
reported for older community-dwelling adults who do not have a
history of stroke. Up to 28% of people with chronic stroke who
experience a fall report sustaining an injury as a result of the
fall (2).
After having a stroke, patients typically undergo a substantial
amount of rehabilitation to decrease impairments and regain
function. One of the many focuses of physical therapy is improving
balance in attempt to reduce the risk and incidence of falls.
Physical therapy interventions to improve balance may include what
are considered “traditional interventions” (i.e. neuromuscular
facilitation, stretching and strengthening exercises, weight-bearing
or shifting activities, exercises on rocker-boards, progressive
challenges in stance, and ADL training) or the use of computer
dynamic posturography (CDP). The SMART EquiTest Balance Master is
one specific CDP machine and will be examined in this article.
In order to reduce the incidence and risk of falls and promote
safety in patients following a CVA, it is important for physical
therapists to be informed on what intervention is most effective in
improving balance. Therefore, the purpose of this article is to
examine whether the Balance Master is more effective than
traditional physical therapy interventions in improving balance in
individuals post-stroke who are at risk for falls.
SMART Balance Master
 The
SMART Balance Master, is a product of NeuroCom International
Inc. The system is comprised of an 18” x 18” dual force
plate that has rotation & translation capabilities to measure the
vertical forces exerted by the user’s feet. The force plate is
contained in a moveable visual surround. The system incorporates all
three components of computerized
dynamic posturography: sensory, motor, and central adaptation, and
has both assessment & retraining capabilities (3).
The
SMART Balance Master, is a product of NeuroCom International
Inc. The system is comprised of an 18” x 18” dual force
plate that has rotation & translation capabilities to measure the
vertical forces exerted by the user’s feet. The force plate is
contained in a moveable visual surround. The system incorporates all
three components of computerized
dynamic posturography: sensory, motor, and central adaptation, and
has both assessment & retraining capabilities (3).
 The assessment protocols consist of the Sensory Organization Test
(SOT), the Adaptation Test (ADT), and the Motor Control Test (MCT)
(4).
The SOT can be used to identify the primary system of balance
impairment: somatosensory, vestibular, or visual. During this test,
six different stages are performed. Each stage isolates and tests a
particular sensory component of balance. Results from the stages can
be found in a printable version of the “Equilibrium Score” graph. The amount of bars under each number on the
x-axis represents the number of trials the participant performed in
each stage of the test. A green bar signifies that a trial was
successfully completed at or above the average COG stability for the
participants’ age, sex, height, and weight. A red bar signifies that
the trial was below average or that a fall occurred during the
trial. A fall consists of taking a step, touching the walls of the
Balance Master, or needing assistance from the physical therapist.
The “Composite” score of the “Equilibrium Score” averages the
results from the six stages and determines if the patient is above
or below the average balance scores for persons of their age and
anthropometrics. The “Sensory Analysis” graph
illustrates the results from the “Equilibrium Score” in terms of the
primary sensory system of balance utilized from the perspective
stages of the test and compares the results to the norm. A red bar
in this graph states that there is a particular sensory deficiency
with this patient but does not diagnose the deficiency or state
exactly where it is located. The “Strategy Analysis” and “COG
Alignment” in the figure demonstrate what average percentage of
balance was due to hip/ankle strategy and where the participants’
average COG alignment was during the six stages (5). (Click on image
for a larger view)
The assessment protocols consist of the Sensory Organization Test
(SOT), the Adaptation Test (ADT), and the Motor Control Test (MCT)
(4).
The SOT can be used to identify the primary system of balance
impairment: somatosensory, vestibular, or visual. During this test,
six different stages are performed. Each stage isolates and tests a
particular sensory component of balance. Results from the stages can
be found in a printable version of the “Equilibrium Score” graph. The amount of bars under each number on the
x-axis represents the number of trials the participant performed in
each stage of the test. A green bar signifies that a trial was
successfully completed at or above the average COG stability for the
participants’ age, sex, height, and weight. A red bar signifies that
the trial was below average or that a fall occurred during the
trial. A fall consists of taking a step, touching the walls of the
Balance Master, or needing assistance from the physical therapist.
The “Composite” score of the “Equilibrium Score” averages the
results from the six stages and determines if the patient is above
or below the average balance scores for persons of their age and
anthropometrics. The “Sensory Analysis” graph
illustrates the results from the “Equilibrium Score” in terms of the
primary sensory system of balance utilized from the perspective
stages of the test and compares the results to the norm. A red bar
in this graph states that there is a particular sensory deficiency
with this patient but does not diagnose the deficiency or state
exactly where it is located. The “Strategy Analysis” and “COG
Alignment” in the figure demonstrate what average percentage of
balance was due to hip/ankle strategy and where the participants’
average COG alignment was during the six stages (5). (Click on image
for a larger view)
 The Balance Master also determines effectiveness of balance during
unexpected movement of the patient’s surroundings. It does this
through the mobile force plate. During this test, known as the
Adaptation Test, the force plate will move suddenly to create dorsiflexion or plantar flexion at the ankle and the patient will
need to use ankle, and potentially hip, strategies to maintain
balance. The force plate is able to gather relevant information
about the amount of ankle force that the patient uses to maintain
balance, as well as the amount of postural sway the patient exhibits
due to the perturbation. These findings can be available in a
printable format as seen here. Like the graphic
representation of the SOT, green figures in the Adaptation Test
represent successful completions of the trial whereas red signify a
fall. The vertical axis of the top two graphs represents ankle force
while the horizontal axis depicts the trial number. The line graphs
in the middle and on the bottom of the figure illustrate the movement
of the participant’s center of gravity along with the direction in
which the ankle force was generated during testing (6). (Click on
image for a larger view)
The Balance Master also determines effectiveness of balance during
unexpected movement of the patient’s surroundings. It does this
through the mobile force plate. During this test, known as the
Adaptation Test, the force plate will move suddenly to create dorsiflexion or plantar flexion at the ankle and the patient will
need to use ankle, and potentially hip, strategies to maintain
balance. The force plate is able to gather relevant information
about the amount of ankle force that the patient uses to maintain
balance, as well as the amount of postural sway the patient exhibits
due to the perturbation. These findings can be available in a
printable format as seen here. Like the graphic
representation of the SOT, green figures in the Adaptation Test
represent successful completions of the trial whereas red signify a
fall. The vertical axis of the top two graphs represents ankle force
while the horizontal axis depicts the trial number. The line graphs
in the middle and on the bottom of the figure illustrate the movement
of the participant’s center of gravity along with the direction in
which the ankle force was generated during testing (6). (Click on
image for a larger view)
Tests within the MCT protocol of the Balance Master include limit of
stability, unilateral stance, weight bearing squat, and weight-shift
tests. The results of each assessment protocol, SOT, ADT, and MCT,
provide objective data which can be referred back to at a later date
to determine balance improvement. These results can also provide
objective data, upon which physical therapy goals and treatment
ideas can be established. Using these assessment protocols, the
Balance Master has been found to be reliable and valid in the
assessment of dynamic balance in stroke patients (7).
The retraining capability of the Balance Master uses functional
training exercises along with sensitive, real time visual feedback
of movement. The clinician is able to adjust the proprioceptive/sensory-motor
and visual training by changing the movement of the support surface,
visual surround, or both to one of three settings: responsive,
variably responsive, or random. In the responsive setting, the
support surface or visual surround move in response to movement of
the patient. The degree of movement of the support surface or visual
surround in the variably responsive setting varies each time the
patient moves. In the random setting, the movement of the support
surface and visual surround is determined by the computer and is not
in response to movement of the patient. The degree of movement is
completely random (3).
Balance Master as the Gold Standard
The Balance Master stands at the forefront of current research. It
has been used as the standardized assessment of balance in the study
of fall prediction in the elderly (8), the effect of AFOs on balance
(9),
the effect of exercise on knee proprioception (10), the relationship
between gait and balance in people with Parkinson’s disease (11), and
the assessment of balance in people with chronic stroke. These
studies, along with others, utilize the Balance Master as the “gold
standard” of balance assessment. But, use of the Balance Master
extends beyond research and is integrated within the hospital and
clinical settings for those that have the financial means to invest
in the system. In fact, the NeuroCom systems are used in 14 of the
17 “Honor Roll” hospitals in the United States according to U.S.
News & World Report, Best Hospitals 2007 (12). This is likely due to
versatility and comprehensive objective data collection as well as
the reliability, responsiveness, and predictive validity that the
Balance Master provides. According to a study of chronic stroke
patients by Chein (13), the equilibrium score (part of the SOT) and the
limits of stability test of the Balance Master had moderate to high
reliability, acceptable responsiveness, and substantial predictive
validity of ADL function. The only aspect of the Balance Master that
did not support its use, according to Chien (13), was the inconsistent
reliability, responsiveness, and predictive variability scores of
the weight-shifting tests.
We have chosen to focus this article specifically on the Balance
Master because it is the gold standard of CDP. Although, the Balance
Master has been well studied in its ability to assess balance, its
ability in retraining balance, specifically in patients post-CVA,
has not received as much publicity. The remainder of this article will
focus on the literature that has emerged regarding the training
capabilities of the Balance Master, and whether it is more effective
than conventional therapy in retraining balance and decreasing falls
during stroke rehabilitation.
Retraining Capabilities of the Balance Master
The literature reviewed showed that although training with the
Balance Master did improve both static and dynamic balance, the
results were not significantly better than those who received
conventional physical therapy. In the articles, static
stability/balance was always tested in a variety of conditions. The
conditions were static stance with eyes open, eyes closed, sway
vision, and sway surface. Pso-Tsai Cheng et al found an improvement
of maximal stability when comparing a Balance Master group to a
control group. However, this difference was not statistically
significant (14). In another clinical update, Deborah Nichols found
that for static stability, biofeedback protocols such as the Balance
Master “may not be any more beneficial than traditional approaches
in increasing postural steadiness, but may add variability of
practice to treatment sessions (15).” Walker et al found that using the
Balance Master did improve patients’ static balance, however, not
any more than the other groups that received physical therapy, or
physical therapy and balance training (16). Finally, Chang Gung found
that the trained group had improvements in static stability at the 6
month follow-up. At the follow-up, the patients were able to use
more ankle strategies, and the amount of displacement of center of
gravity decreased when compared to the control group. However, as in
the other studies, there was no statistically significant
difference (17).
In the articles, dynamic balance was seen to improve, though not
always more than the control groups. Dynamic balance was usually
measured by examining how close patients could get to their limits
of stability (LOS), as well as how fast they could move from one
target to another. Gung found significant improvements in dynamic
balance at the 6 month follow up. Patients had an increased axis
velocity from 3.25 degrees/second to 4.11 degrees/second. Patients
were able to get closer to their LOS and had better directional
control. Pao-Tsai Cheng et al also agreed with this conclusion. This
group found significantly improved dynamic balance at initial
training and at the 6 month follow-up. For on-axis velocity, the
training group increased from 3.19 degrees/second to 4.08
degrees/second at the end of treatment, and to 4.11 degrees/second
at the 6 month follow up (14). Walker et al found improvement in
dynamic balance, but at the same rate as the control group. They
state that it is “conceivable that the regular therapy sessions
alone sufficed to enable patients to maximize their potential (16).”
Additionally, the visual feedback provides patients with constant
feedback. While this feedback may be beneficial during training,
patients may become too dependent on it, and lose their ability to
self-correct when the visual feedback is not available. Nichols
found that weight-shifting tasks that can be performed on the
Balance Master improved “accuracy of weight shift” in a variety of
subjects, including older subjects with and without balance issues
as well as subjects with hemiparesis (15). However, Nichols does note
that “in cases where feedback training and testing protocol [are]
similar, the ability to distinguish between performance and learning
was limited (16).”
In addition to looking at static and dynamic balance, several of the
studies also looked at outcome measurements, which overall did not
show improvements between groups. Using the FIM, Gung looked at mean
changes of self-care, sphincter control, locomotion and mobility
functions. Gung identified that there was improvement in all these
areas, but only self-care had statistically significant difference
at the 6 month follow up. The authors also noted that using the
Balance Master “seemed to be more correlated with the ability to
perform self-care tasks than locomotion and mobility function (17).”
Walker et al looked at balance based on activity type. The three
tests used were the Berg, the Timed “Up and Go” test (TUG test), and
gait speed. While the authors did find improvements in all their
scores, there were no differences between the three groups for any
outcome measure overtime. This indicates equivalency in balance
performance regardless of differences in intervention. Walker notes
that all gains were greatest during the inpatient period and that
standard treatment along with spontaneous recovery may be enough to
maximize patients’ potential (16). Finally, a randomized control trial
by Greiger et al examined training with the Balance Master in
addition to conventional physical therapy to improve balance and
mobility as measured by the Berg Balance Scale and the Timed “Up and
Go” Test. When compared to a control group receiving conventional
physical therapy, the addition of training with visual biofeedback
and a forceplate system (e.g. Balance Master) resulted in no
differences between the groups after 4 weeks of intervention.
However, the mean difference scores for the entire population of the
study did not correlate to each other. This suggests that some
subjects made greater gains on one measure than on the other.
Furthermore, the study may have had a type II error as it only
contained 13 subjects (18).
The majority of the articles reviewed did not directly study whether
there was a difference in the incidence of falls between the Balance
Master groups and the control groups. However, some theorized that
there would be a decrease in the risk of falls if there were
improvements in other tasks. Gung states that using the
weight-shifting tasks done in their study may be helpful in
improving stance symmetry, but did not relate it to better gait or
other high level balance or mobility tasks (17). Nichols et al found
that by using the Balance Master, subjects were able to expand their
limits of stability. In theory, Nichols believes this should
decrease the likelihood of falling, but at the time of their study
this relationship had not been examined (15). One article that did look
at the occurrence of falls was that by Pao-Tsai Chung et al. This
group relied on self-reporting from patients at the 6 month follow
up. The group found that the occurrence of falls in the training
group was lower than that of the non-trained group (17.8% vs.
41.7%). However, this difference was not statistically significant.
The authors feel this may be a result of a small sample size (14).
Conclusion
Balance disturbances are one of the biggest issues that stroke
patients deal with, in turn it is essential to determine the best
form of evaluation and treatment for these same individuals (1). Recent
studies show that NeuroCom’s Balance Master is currently the gold
standard for assessment of balance, especially in individuals who
have had a CVA. The Balance Master provides objective data allowing
clinicians to document and making it easier for these clinicians to
show improvement in patients. The Balance Master is also being used
for retraining after strokes in order to improve static and dynamic
balance, improve gait, and decrease the risk of falls. Recent study
results have shown that using a balance master during therapy is no
more beneficial than standard post-stroke rehabilitation when
looking at a patient’s improvements in balance. Across the board,
studies found that there is generally an improvement in balance
after training, but it is not a statistically significant difference
when comparing to a control group who receives the traditional
therapy.
Many major hospitals in the United States have instituted the use of
the Balance Master in agreement with the fact that studies have
shown that it is currently the gold standard for balance assessment.
Further testing is necessary however, to determine if the Balance
Master is any better than conventional physical therapy after stroke
for improving balance and gait or decreasing the risk of falls. At
this time, study results show no significant difference between
conventional PT and using the Balance Master when it comes to
balance improvements post-stroke.
Last revised: September 10, 2009
by Katie Nitsch-Pachniak, DPT
References:
1. O’Sullivan SB. Stroke. In: O’Sullivan SB, Schmitz TJ.
Physical Rehabilitation. 5th ed. Philadelphia, PA: F.A. Davis Company; 2007:
705-769.
2. Harris JE, Eng JJ, Marigold DS, Tokuno CD, Louis CL. Relationship of
Balance and Mobility to Fall Incidence in People with Chronic Stroke.
Physical Therapy. 2005; 85(2): 150-158.
3. NeuroCom International Incorporated. The SMART EquiTest page. Available
at:
http://resourcesonbalance.com/neurocom/products/SMARTEquiTest.aspx.
Accessed September 14, 2009.
4. Hackney J, Torgersen R. Inservice. Balance Master Inservice. All Saints
Hospital, Racine, Wisconsin.
5. NeuroCom International Incorporated. NeuroCom Protocols: Sensory
Organization Test page. Available at: http://ncmseminars.com/neurocom/protocols/sensoryImpairment/SOT.aspx.
Accessed November 23, 2008.
6. NeuroCom International Incorporated. NeuroCom Protocols: Motor Impairment
Assessments. Available at:
http://ncmseminars.com/neurocom/protocols/motorImpairment/ADTReport.gif.
Accessed September 14, 2009.
7. Liston R, Brouwer B. Reliability and validity of measures obtained from
stroke patients using the balance master (Abstract). Archives of Physical
Medicine and Rehabilitation. 1996; 77(5): 425-430.
8. Alencar MA et al. Muscular function and functional mobility of faller and
non-faller elderly women with osteoarthritis of the knee. Brazilian Journal
of Medical & Biological Research. 2007; 40(2):277-83.
9. Chen CK et al. Effects of an anterior ankle-foot orthosis on postural
stability in stroke patients with hemiplegia. American Journal of Physical
Medicine & Rehabilitation. 2008; 87(10):815-20.
10. Subasi SS et al. Effects of different warm-up periods on knee
proprioception and balance in healthy young individuals. Journal of Sport
Rehabilitation. 2008; 17(2):186-205.
11. Yang YR et al. Relationships between gait and dynamic balance in early
Parkinson's disease. Gait & Posture. 2008; 27(4):611-5.
12. NeuroCom International Incorporated. More About NeuroCom International,
Inc. page. Available at: http://www.onbalance.com/aboutNCM.php. Accessed
November 18, 2008.
13. Chien CW et al. A comparison of psychometric properties of the smart
balance master system and the postural assessment scale for stroke in people
who have had mild stroke. Archives of Physical Medicine & Rehabilitation.
2007; 88(3):374-80.
14. Pao-Tsai Cheng et al. Effects of Visual Feedback Rhythmic Weight-shift
Training on Hemiplegic Stroke Patients. Clinical Rehabilitation. Vol. 18,
No. 7. 2004. pp. 747-753.
15. Nichols DS. Balance Retraining After Stroke Using Force Platform
Biofeedback. Physical Therapy. Vol. 77, No. 5, May 1997, pp. 553-58.
16. Walker C, Brouwer BJ, Culham EG. Use of Visual Feedback in Retraining
Balance Following Acute Stroke. Physical Therapy. Vol. 80, No. 9, September
2000, pp. 886-95.
17. I-Chun Chen et al. Effects of Balance Training on Hemiplegic Stroke
Patients. Chang Gung Med J. 2002; 25: 583-90. Available at: http://cgmh.org.tw/cgmj/2509/250903.pdf.
Accessed September 14, 2009.
18. Geiger Ra et al. Balance and Mobility Following Stroke: Effects of
Physical Therapy Interventions With and Without Biofeedback/Forceplate
Training. Physical Therapy. Vol. 81, No.4, April 2001, pp. 995-1005.


 According
to O’Sullivan, a stroke or cerebral vascular accident (CVA) is
defined as a sudden loss of neurological function caused by an
interruption in blood flow to the brain with neurologic deficits
persisting for greater than 24 hours. Strokes cause damage to brain
tissue. Clinical manifestations include changes in consciousness and
impairments in sensation, motor function, cognition, perception, and
language (1).
According
to O’Sullivan, a stroke or cerebral vascular accident (CVA) is
defined as a sudden loss of neurological function caused by an
interruption in blood flow to the brain with neurologic deficits
persisting for greater than 24 hours. Strokes cause damage to brain
tissue. Clinical manifestations include changes in consciousness and
impairments in sensation, motor function, cognition, perception, and
language (1).







