|
PT Classroom - Neutral in Context: Not in Gait ׀ by Edward S. Glaser, DPM |

Edward Glaser, DPM, studied mechanical engineering at SUNY at Stonybrook, and went on to receive his doctorate in podiatric medicine at the New York College of Podiatric Medicine. This is not a common pathway for a medical student, but it turned out to be just the right exposure for a future student of the foot. He was in private practice for 13 years before dedicating all of his energies to the development of his MASS Position Theory and Orthotic Design, which has added a new and comprehensive paradigm to the field of biomechanics. He has earned a substantial national and international reputation for re-visioning and re-engineering the way practitioners can significantly correct poor biomechanics in the foot and lower extremity. His new analysis and practical, common-sense approach to the casting and design of custom, full arch contact, calibrated foot orthotics has helped many health care providers achieve a new level of clinical success. He offers the first credible challenge to the standard, industry techniques originated by Root, Orien and Weed in 1977. |
The Rootian Revolution in the late 1970’s brought a much needed focus on foot biomechanics, especially the need to improve or manage it in the individual patient. While Root et al did an admirable job analyzing normal and abnormal foot function(7), justifiably establishing their preeminence in the field, they did a curious thing when it came to intervention strategy. Without the rigorous guidance of research, they proposed the now mainstream orthotic methodology of casting in “neutral” and posting under the rearfoot(8). Such is the power of notoriety and perceived expertise to dictate common practice.
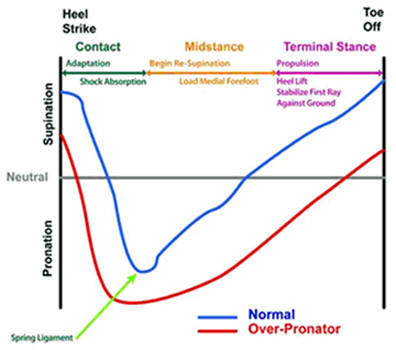
If we try, though, to find the relevance of “neutral” to healthy stance-phase gait, we immediately run into significant problems(1-6, 9,10). No one seems to be able to connect the neutral model of correction to what should be happening in gait. This is certainly true when we look at the functional problems of the flexible over-pronator. In this article we outline six functional goals on which the casting and design of truly effective orthotics should be based.
1. Sufficient supination at heel strike. Pronation will
proceed more rapidly and deeply if the foot arrives pre-pronated
on the ground. This is because the subtalar joint requires a
tightly-nested, i.e. supinated, posture to resist rapid
unraveling towards pronation.
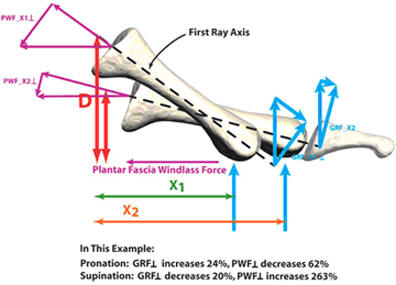
There are three main forces during midstance that are pertinent to achieving re-supination for push-off: 1) The ground reactive force in the pronated foot has a greater lever arm to cause further pronation. 2) The re-supination torque of the windlass effect has a greater lever arm to facilitate supination if it starts from a supinated position. 3) Leg external rotation, the re-supination force of which is facilitated by starting from a less pronated position. A simple way to think about this is that the supination resistance is less when the foot is less pronated and increases dramatically when it is in full pronation11. The determination of how much supinatory force is required is central to the decision making process in the prescription of custom foot orthoses.
In light of these goals, where does neutral position correction have an impact? Neutral methodology calls for at least 50% pronation of the subtalar joint and maximum pronation of the midtarsal joints. Clearly, we need to facilitate significantly more supination than this if the foot is to achieve the above goals. Neutral methodology assumes that a rearfoot post is able to influence calcaneal inversion in the instant of heel strike. That this is a mechanical impossibility we will explore in future articles. Then, as the heel lifts off the ground, how do we facilitate re-supination when the post makes no forcible contact with the heel? These are the issues that beg for a new model of correction. We will begin to explore this new model in future articles.
Last revised: October 1, 2008
References: |
|
|
|
|