Nearly one-third of Americans age 30-70 experience
bladder control symptoms at some point. Nearly 64% of those never seek
treatment. In addition, women wait, on average, 6.4 years to seek treatment,
while men wait 4.2 years (1). Out of 1,961 non-pregnant healthy women, 23.7%
experienced urinary or fecal incontinence, pelvic organ prolapse, or in
combination (2). Thirty eight percent of men and women believe that incontinence
is a normal sign of aging (1).Estimates range that 80% of those with incontinence
can be cured, or at least improved, by conservative treatments.
Ten percent of women ages 20-39, 27% ages 40-59, 37% ages 60-79, and 50% ages
80+ experience urinary incontinence.
What is pelvic floor physical therapy?
Pelvic floor physical therapy is a subset of physical therapy that involves
evaluation of the pelvic floor, which is a group of muscles that supports the
pelvic organs. These pelvic organs include the bowel, bladder, and the uterus in
women. This can include either vaginal or colorectal examination and treatment.
What is the Pelvic Floor?
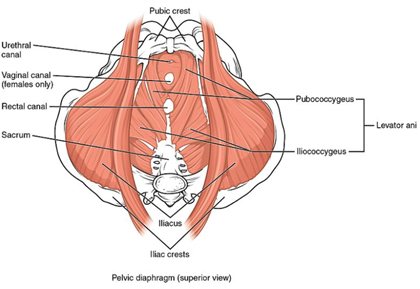
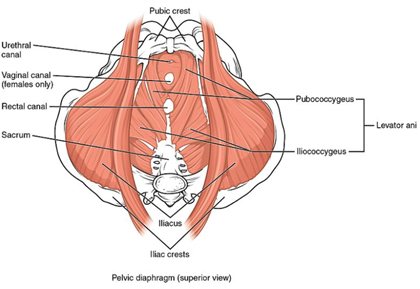
The pelvic floor is comprised of a group of muscles,
ligaments, and connective tissue structures that provide
support to visceral organs, resist intra-abdominal
pressure, maintain urinary and fecal continence, and
provide various sexual functions. The levator ani group
and coccygeus muscles make up the deep pelvic floor
(layer three) that act like a hammock or sling. The
rectum, urethra, and vagina all pass through the pelvic
floor; dysfunction in any of the pelvic floor muscles
can affect one or more of these structures (4-6).
The pelvic floor is comprised of 3 layers of muscles:
Superficial Perineum (layer 1)
1. Bulbocavernosus
2. Ischiocavernosus
3. Superficial transverse perineal
4. External anal sphincter (EAS)
Deep Urogenital Diaphragm (layer 2)
1. Compressor urethera
2. Uretrovaginal sphincter
3. Deep transverse perineal
Pelvic Diaphragm (layer 3)
1. Levator ani: pubococcygeus (pubovaginalis,
puborectalis), iliococcygeus
2. Coccygeus/ischiococcygeus
3. Piriformis
4. Obturator internus
Common Diagnoses That Are Treatable with Pelvic
Floor Physical Therapy
Dysfunction in any of the above muscles can lead to
pelvic pain, urinary or fecal incontinence, symptoms of
prolapse, or a combination. Below are a few diagnoses
that are commonly addressed in pelvic floor PT:
• Pelvic pain, including pain with intercourse or pelvic
exam
o Dyspareunia: difficult or painful sexual intercourse
o Vaginismus: involuntary contraction/spasm of pelvic
floor muscles
o Vulvodynia: chronic pain surrounding the introitus
o Endometriosis: endometrial tissue growth on other
pelvic structures (i.e. ovaries, bowel, lining of pelvic
structures)
o Pudendal neuralgia: chronic pelvic pain from
irritation/damage to the pudendal nerve
o Interstitial cystitis/painful bladder syndrome:
chronic condition causing bladder pressure, bladder pain
and sometimes pelvic pain
• Pelvic organ prolapse
• Urinary leakage with or without activity
• Urinary frequency or urgency
• Diastasis recti (separation of abdominal muscles
• Abdominal pain or scar tissue associated with
abdominal or pelvic surgery
• Trauma/PTSD
• And many more!
Can’t we just prescribe Kegels to all of our pelvic
floor patients?
NO! There are two general diagnoses for various pelvic
floor dysfunctions:
1. Overactive/functionally short pelvic floor
2. Underactive/weak pelvic floor
Even when kegels are indicated, an American Journal of
Obstetrics and Gynecology research article states that
up to 51% of individuals do not perform a kegel
correctly (3).
Pelvic Floor Evaluation & Treatment
The initial evaluation for a pelvic floor patient is
very similar to a patient with lumbopelvic dysfunction.
Posture, gait, spinal mobility, lower extremity
flexibility and strength, transverse abdominis
stabilization, joint accessory motion, and special tests
including lumbar/sacroiliac joint dysfunction and load
transfer tests are all appropriate. In addition, pelvic
floor PTs perform an internal and external assessment of
the pelvic floor region, including skin integrity and
scar mobility, sensation, pelvic floor contractile
strength and endurance, internal and external soft
tissue quality/irritability, and assessment for prolapse
(just to name a few!).
If the patient is found to have an underactive pelvic
floor, pelvic floor strengthening interventions will be
utilized for improved strength and control of the pelvic
floor and presenting symptoms. If the patient is found
to have an overactive pelvic floor (i.e. pelvic pain,
some stress incontinence), pelvic floor relaxation and
downtraining interventions will be implemented for
decreased resting tone of the pelvic floor.
Common treatments for pelvic floor dysfunction
include pelvic floor strengthening or relaxation
strategies, internal and external soft tissue
mobilization, electrical stimulation for pain
management/muscle stimulation, sEMG biofeedback for
neuromuscular re-education, spinal and neural
mobilizations, dynamic hip strength and transverse
abdominis stabilization, lower extremity stretching,
education in proper mechanics and behavioral strategies,
and a comprehensive home exercise program. Keep in mind
that not all of these interventions are appropriate for
every patient, and are to be utilized based on objective
findings from the initial evaluation.
Last revised: 4/18/19
by Emily Schwecke
References
1) Muller, Nancy. What Americans Understand and How They
Are Affected by Bladder Control Problems: Highlights of
Recent Nationwide Consumer Research. Society of Urologic
Nurses and Associates. 2005:25(2): 109-115.
https//www.suna.org/download/members/unjarticles/2005/05apr/109.pdf.
2) Nygaard, I. Barber, M. Burgio, K. Kenton, K. Meikle,
S. Schaffer, J, et. al. Prevalence of Symptomatic Pelvic
Floor Disorders in US Women. JAMA. 2008:300(11):
1311-1316.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2918416
3) Bump, RC. Hurt, WG. Fantl, JA, Wyman, JF. Assessment
of Kegel pelvic floor exercise performance after brief
verbal instruction. Am J Obstet Gynecol. 1991:165(2):
322-7 https://www.ncbi.nlm.nih.gov/pubmed/1872333
4) Corton MM. Anatomy of pelvic floor dysfunction.
Obstet Gynecol Clin North Am. 2009;36(3):401-419.
5) Herschorn S. Female pelvic floor anatomy: the pelvic
floor, supporting structures, and pelvic organs. Rev
Urol. 004;6(suppl 5):S2-S10.
6) Pelaez M, Gonzalez-Cerron S, Montejo R, Barakat R.
Pelvic floor muscle training included in a pregnancy
exercise program is effective in primary prevention of
urinary incontinence: a randomized controlled trial.
7) Allen T, Real J. Herman & Wallace Level 2B: Pelvic
Floor Function, Dysfunction, and Treatment. Lecture
Presented: Rehabilitation of Pelvic Pain; May 18-20th,
2018; Kenosha, WI.