|
Game On….
Rehabilitation Strategies for Post Concussion
Syndrome |
 Many
victims of concussion injuries report signs and symptoms
years after the incidents. In a recent study (2014 and
2015), a team of physical therapists and allied health
professionals discovered that specific manual therapy
techniques produced significant results toward the future of
concussion recovery. The patients in the study were retired
professional football players from both the National
Football League (NFL) and the Canadian Football League (CFL)
with post concussion syndrome. These initial outcomes are
inspiring and show real promise for viable treatment options
for Traumatic Brain Injury (TBI), concussion, and the
secondary compensatory dysfunctions that take place in the
days following brain injury. Many
victims of concussion injuries report signs and symptoms
years after the incidents. In a recent study (2014 and
2015), a team of physical therapists and allied health
professionals discovered that specific manual therapy
techniques produced significant results toward the future of
concussion recovery. The patients in the study were retired
professional football players from both the National
Football League (NFL) and the Canadian Football League (CFL)
with post concussion syndrome. These initial outcomes are
inspiring and show real promise for viable treatment options
for Traumatic Brain Injury (TBI), concussion, and the
secondary compensatory dysfunctions that take place in the
days following brain injury.
In 2012, a group of concerned physical therapists were
meeting for a common desire to help improve the quality of
life that people experience following brain injury or
concussive impacts. We wanted to emphasize that the injured
person was “not alone” in their road back to recovery. We
wondered if the years of study and the specific techniques
that we have trained in would benefit patients who had
suffered concussions. At that time, our colleagues were
devastated by the recent loss of lives due to the severity
of symptoms the retired football players were dealing with,
and the diagnosis of Chronic Traumatic Encephalopathy (CTE).
As our curiosity grew, so did the desire to design a
research project to determine if our techniques and passion
to help would prove beneficial. We were aware of the 2011
study that Dr. Amen (et al) had published as the first and
largest brain imaging study (SPECT and Quantitative EEG) of
100 active and retired NFL players. They reported consistent
damage to the brain’s prefrontal cortex (judgment, impulse
control), temporal lobes (memory, mood stability), parietal
(spatial orientation), occiput (visual field), and the
cerebellum (mental agility, coordination, speed). (1) In
2013, after the death of retired NFL linebacker, Junior
Seau, the compassion from fellow colleagues encouraged us to
pursue our study.
Could the techniques of Upledger CranioSacral Therapy,
Barral Visceral Manipulation, and Barral Neural Manipulation
help the biochemical and structural changes that occur after
TBI/Concussive injuries?
Could these advanced manual therapy techniques somehow
assist the natural healing process that should occur after
tissues have been damaged?
Could we assist the brain and nervous system toward
recovery, and therefore neuroplasticity (ability for the
brain to regain homeostasis via appropriate stimulatory
factors)?
Could this method of treatment be an integral step in the
rehabilitation strategies of the concussive patient?
Our curiosity prevailed and we were given an opportunity to
find out some answers to these questions. The Dr. John E.
Upledger Foundation in Palm Beach Gardens, Florida and
the Ricky Williams Foundation in Texas provided a platform
to begin our Concussion Pilot Program (CPP). The CPP team
consisted of a medical director, a research director, a
program coordinator, a psychotherapist, and a team of highly
qualified therapists who had been selected from around the
world by the Upledger Institute International in conjunction
with the foundations. We were all there to embrace the
spirit of hope and represent a true team approach, which is
so vital to recovery.
In the earlier days of sports injuries, there was no clear
strategy for treating concussions. Care improved as the
medical profession gained more experience with the clinical
signs and symptoms. Acute assessment and daily symptom
evaluation by the trainers, possible referral to a
physician, home management instructions, and abstention from
doing any activity that caused the symptoms to increase
became the protocol. With the continued complaints from
patients in our offices and the continued complaints we read
about from other professionals, it was becoming more
apparent that this protocol was not enough intervention for
the intensity of dysfunction that occurred around a
concussive injury.
The professionals involved with this study have had many
collective years of experience working with patients having
TBI, Autism, PTSD, Anxiety, Depression, Chronic Headache,
Chronic Pain, Memory Loss, and Sleep Disorders. The
treatment modalities used were developed in the mid 1970’s,
so a 40-year history of clinical expertise exists.
Upledger CranioSacral Therapy
(CST) is a light touch whole body treatment that works by
freeing restrictions within the deeper fascial system that
supports and surrounds the central nervous system. CST
focuses on glial cells, which are the supporting matrix of
the structures of the brain (like fascia), the cranial
bones, and the connective tissues inside these bones. (2)
Barral Visceral Manipulation
(VM) is a gentle manual therapy that assesses the structural
and functional relationship between the organs, and their
fascial or ligamentous attachments to the various systems in
the body. VM assists the release of restrictions found
within these relationships, such as musculoskeletal,
vascular, digestive, eliminatory, respiratory, lymphatic,
and the autonomic nervous system. (3)
Barral Neural Manipulation
(NM) focuses on releasing local nerve restrictions within
the central and peripheral nervous systems. It is also a
lighter touch manual therapy that examines how the release
of these local nerve fixations resolves the more
comprehensive (global) dysfunctional patterns. (4)
In summary, these modalities are capable of accessing and
addressing the structural, vascular, and neurological
tissues of the cranium and brain, as well as the
far-reaching ramifications throughout the body.
The CPP design consisted of five consecutive days of
treatment. Each participant received a therapy session in
the morning and another in the afternoon. Each participant
had an initial evaluation in the morning of Day One, a post
evaluation in the afternoon of Day Five, and then a follow
up evaluation in three months. The testing methods consisted
of:
MD evaluation
Impact Neurocognitive Test
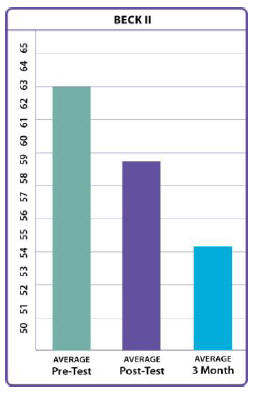
Beck II Depression Inventory (BDI)
SF36 Quality of Life Test
Headache Impact Test (HIT-6)
Dizziness Handicap Inventory (DHI)
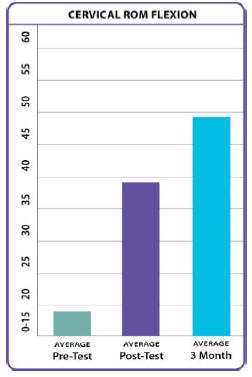
Range of Motion tests for the involved joints, as well as
the cervical and lumbar regions
Vestibular testing
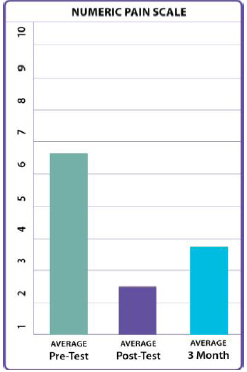
Numeric Pain Scale testing
Quality/hours of sleep
Our first goal was to explain to the participant what might
be happening within their bodies as we became acquainted
with their individual patterns of dysfunction. Recent
studies in neuroscience have discovered when working with
trauma, an important step in the healing process occurs when
a person has a better understanding of their personal
situation (self awareness/mindfulness). (5)
Our next goal was to calm the threat felt by the nervous
system that is overwhelming the coping mechanism for
handling trauma. Our final goal was to break the pattern of
excessive nerve firing, vascular insufficiency, autonomic
responses, anxiety related to these stressors,
sleeplessness, inflammation, and muscle tensions. All of
these issues were leading to the chronic pain, fatigue,
dizziness, headaches, depression, memory loss, and quality
of life issues that were complaints of these participants.
The number of concussions for each participant ranged from 3
– 100, with loss of consciousness reported in 6 out of the
11 retired players. We had five participants in the 2014
study and six participants in the 2015 study. Their ages
ranged from the mid 20’s to the mid 50’s.
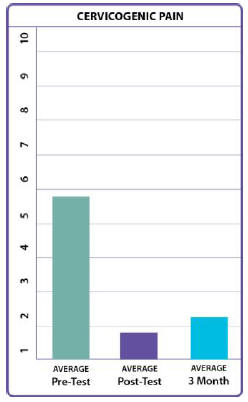
The results show a significant decrease in depression and
their overall pain scales. They had a significant increase
in the number of hours slept per night and in quality of
life issues (general health, bodily pain, energy, emotional
well-being, and social functioning). This group did not come
in with headaches and dizziness being a major problem.
The range of motion within the cervical and lumbar regions,
or with a primary effected joint from previous injuries,
improved immediately and continued to gain in the three
month evaluation. The balance and vestibular testing was
improved, but not as significant as the other findings. In
the neurocognitive tests there was a statistically
significant increase p=0.0156 in their memory scores.
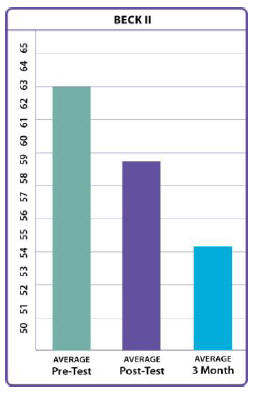
Beck Depression Inventory II (tests symptoms associated with
depression.

SF 36 QoL (Quality of Life)
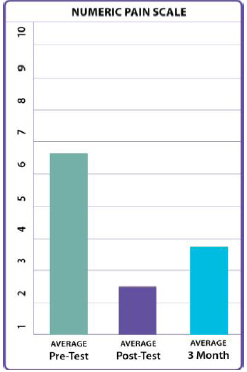
Numeric Pain Intensity Scale (number given by participant for overall pain)

Average Hours of Sleep Per Night
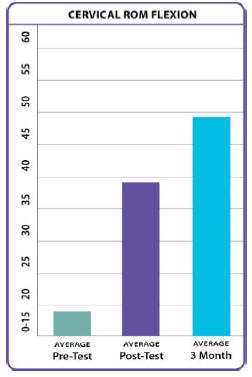
Cervical Range of Motion – Flexion
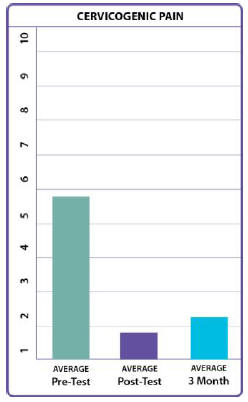
Pain Coming from the Neck Area
We are aware of the fact that this was a small number of
participants for the Concussion Pilot Program, but we would
like to think that the manual therapies presented here may
be worth looking into for further studies. Perhaps we are
looking toward viable treatment options that can be taken
into other clinics for concussion rehabilitation. We are
encouraged by the possibilities specific manual therapy may
be able to provide for the health and healing of concussive
or TBI patients. Perhaps it was the stimulation of increased
blood flow (SPECT scan showed a decrease in blood flow to
certain areas post concussion, which is consistent with the
lasting effects of TBI). (6) Perhaps it was the resolution
of fascial restrictions, or changing extracellular
electromechanical information through integrins (receptors
within the cell membrane). (7) Perhaps it was the increase
in proprioception for structural/functional integration, or
the bringing together of mind, emotions and body awareness.
These initial results are extremely promising, as post
concussion syndrome does not seem to be isolated to the
brain. Our discoveries during the study found that the
autonomic nervous system, the enteric nervous system, and
the vascular/lymph/organ systems have secondary compensatory
dysfunctions that take place within this syndrome, as well.
Each case reported varied and random pain throughout their
body, and each case reported previous joint or muscle pain
that elevated after the concussion.
Could this method of treatment be an integral step in the
rehabilitation strategies for the concussive patient? The
results suggest that we are getting one step closer.
Last revised: February
18,2017
by Gail Wetzler, PT, DPT, EDO, BI-D
References
1. Impact of Playing American Professional Football on
Long-Term Brain Function, Amen,
D., Newberg, A., Thatcher, R., Jin, Y., Wu. J., Keator, M.,
Willeumier, K., Journal of Neuro-
psychiatry Clinical Neuroscience 23:1, Winter, 2011.
2. CranioSacral Therapy, John E. Upledger, D.O., F.A.A.O.
and Jon Vredevboogd, M.F.A.
Eastland Press, 1984.
3. Cell Talk, John E. Upledger, D.O., O.M.M., North Atlantic
Books, 2003.
4. Visceral Manipulation, Jean Pierre Barral, Eastland
Press, 1988.
5. Manual Therapy for the Cranial Nerves, Jean Pierre Barral
and Alain Croibier, Churchill
Livingstone, 2009.
6. The Body Keeps the Score, Van der Kolk, B., Penguin
Books, New York, 2014.
7. PET Imaging for Traumatic Brain Injury, Dubroff, J.,
Newberg, A., PET Clinical 5, 2010,
199-207.
8. The Living Matrix: A Model for the Primary Respiratory
Mechanism, Lee, RP., Explore,
Nov/Dec 2009, Vol. 4 No. 6.
|
 Gail
Wetzler currently owns an integrative physical therapy
practice in Denver, Colorado, where they treat orthopedic,
fascial/muscular/soft tissue, neurologic, pain,respiratory,
digestive, mTBI and women's and men's health issues. After
receiving her initial degree in physical therapy, she
pursued her first experience in acute orthopedic care at
Hoag Hospital, Newport Beach California. Within 1 year, she
became the outpatient clinical supervisor and thus began her
journey and desire for continuing education in the science
and art of human movement and function. She studied with
Travell and Simons, Mennell, Kaltenborn, Maitland, McKenzie,
Mitchell, Jones and Greenman in the earlier years of manual
therapy education. Inspired by these methods of treatment,
she became an assistant teacher to Dr. Janet Travell and
later an instructor with the Institute of Physical Art (IPA)
developed by Gregg Johnson and Vicky Saliba Johnson.
Click here for
full bio
Gail
Wetzler currently owns an integrative physical therapy
practice in Denver, Colorado, where they treat orthopedic,
fascial/muscular/soft tissue, neurologic, pain,respiratory,
digestive, mTBI and women's and men's health issues. After
receiving her initial degree in physical therapy, she
pursued her first experience in acute orthopedic care at
Hoag Hospital, Newport Beach California. Within 1 year, she
became the outpatient clinical supervisor and thus began her
journey and desire for continuing education in the science
and art of human movement and function. She studied with
Travell and Simons, Mennell, Kaltenborn, Maitland, McKenzie,
Mitchell, Jones and Greenman in the earlier years of manual
therapy education. Inspired by these methods of treatment,
she became an assistant teacher to Dr. Janet Travell and
later an instructor with the Institute of Physical Art (IPA)
developed by Gregg Johnson and Vicky Saliba Johnson.
Click here for
full bio
 Many
victims of concussion injuries report signs and symptoms
years after the incidents. In a recent study (2014 and
2015), a team of physical therapists and allied health
professionals discovered that specific manual therapy
techniques produced significant results toward the future of
concussion recovery. The patients in the study were retired
professional football players from both the National
Football League (NFL) and the Canadian Football League (CFL)
with post concussion syndrome. These initial outcomes are
inspiring and show real promise for viable treatment options
for Traumatic Brain Injury (TBI), concussion, and the
secondary compensatory dysfunctions that take place in the
days following brain injury.
Many
victims of concussion injuries report signs and symptoms
years after the incidents. In a recent study (2014 and
2015), a team of physical therapists and allied health
professionals discovered that specific manual therapy
techniques produced significant results toward the future of
concussion recovery. The patients in the study were retired
professional football players from both the National
Football League (NFL) and the Canadian Football League (CFL)
with post concussion syndrome. These initial outcomes are
inspiring and show real promise for viable treatment options
for Traumatic Brain Injury (TBI), concussion, and the
secondary compensatory dysfunctions that take place in the
days following brain injury.